Policy recommendations to improve vaccine acceptance and reduce vaccine hesitancy
The COVID-19 pandemic has caused significant morbidity and mortality globally, across multiple waves. The recent situation in India has been grim. Evidence suggests that the spread of the virus can be mitigated through physical distancing, non-pharmaceutical interventions like use of face masks / shields and maintaining hand hygiene, and in advanced cases of morbidity, therapeutics.
The risk of outbreaks and disruption to societal and economic activity likely remains until effective vaccines are administered to prevent hospitalisation and limit infection. Emerging evidence also suggests that even a single dose of some COVID vaccines reduces infection rates across population groups. Therefore, it is essential to ensure equitable access to vaccines within and across all nations.
Several novel vaccines were developed in rapid response to the urgent need for a long-term solution to curb the spread of COVID 19 infection. Some COVID-19 vaccines have now been authorised or approved for human use, with some in the late stages of clinical development. The speedy rollout of vaccines is essential for complete economic reopening and recovery across the country. The Government of India’s CoWIN portal reported in the last week of April that 150 million doses of vaccine have been administered with 25 million individuals having received both the doses.
Vaccine hesitancy has been reported anecdotally, although the prevalence of this phenomenon remains to be rigorously studied in India, particularly as the second wave mounts. India is phasing this summer into opening vaccines to all adult populations of age group 18 years and above, and vaccine acceptance will be critical.
The Rapid Evidence Synthesis team at the George Institute for Global Health and the Knowledge Management Division (KMD) of the National Health Systems Resource Centre (NHSRC) have collaborated to identify evidence on the determinants of vaccine acceptance and hesitancy, interventions that can promote vaccine acceptance, and also review relevant literature that contextualises this evidence in light of the ongoing pandemic crisis in India.
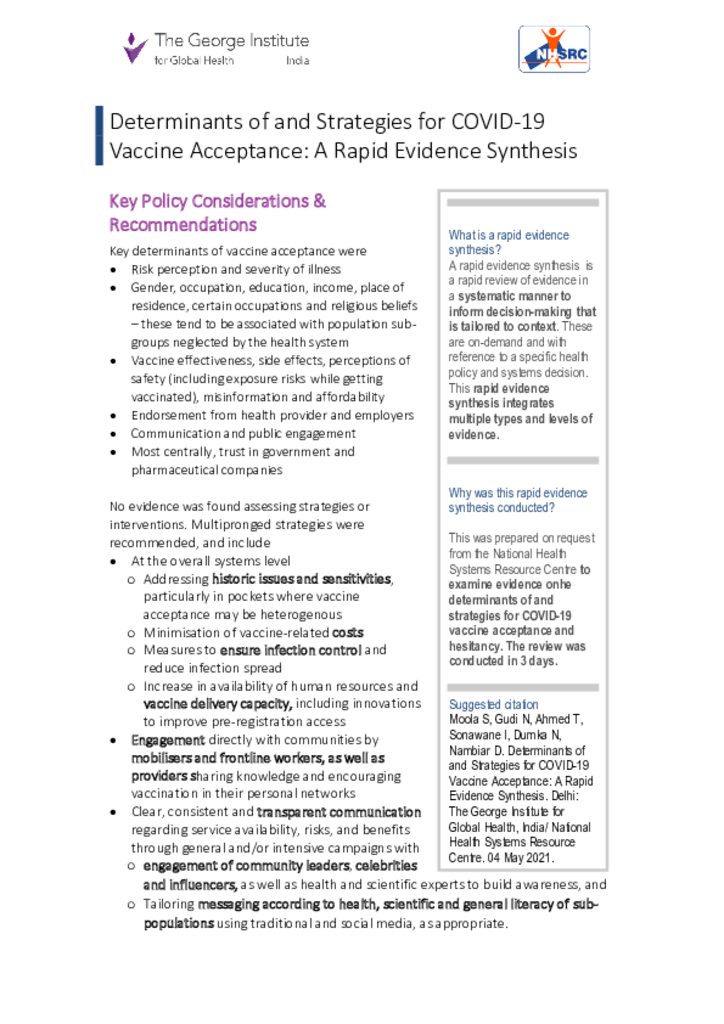
Based on discussions and a scoping brief, this rapid evidence synthesis (RES) addresses the following objectives:
- What are the determinants of COVID-19 vaccine acceptance and hesitancy?
- What interventions have been shown to improve COVID-19 vaccine acceptance and reduce hesitancy?
- What contextual considerations related to the aforementioned are relevant for India’s COVID scenario?
Policy Implications
- This RES lays out evidence from LMICs, including India, in relation to a (WHO) framework to understand COVID vaccine acceptance and hesitancy.
- It contextualises evidence – including from pre-prints- to make recommendations (see below).
- It expands the scope of response to vaccine acceptance and hesitancy beyond vaccine communication strategies, which, as evidence suggests, are necessary, but not sufficient.
Policy Recommendations
Policy makers at national and subnational levels may consider the following key determinants of vaccine acceptance – which likely shape strategies
- Risk perception and severity of illness
- Gender, occupation, education, income, place of residence, certain occupations and religious beliefs – these tend to be associated with population sub-groups neglected by the health system
- Vaccine effectiveness, side effects, perceptions of safety (including exposure risks while getting vaccinated), misinformation and affordability
- Endorsement from health provider and employers
- Communication and public engagement
- Most centrally, trust in government and pharmaceutical companies
No evidence was found assessing strategies or interventions. Multipronged strategies were recommended, and include
- At the overall systems level
- Addressing historic issues and sensitivities, particularly in pockets where vaccine acceptance may be heterogenous
- Minimisation of vaccine associated costs borne by the public
- Measures to ensure infection control and reduce infection spread o Increase in availability of human resources and vaccine delivery capacity, including innovations to improve pre-registration access
- Engagement directly with communities by mobilisers and frontline workers, as well as providers sharing knowledge and encouraging vaccination in their personal networks – in the Indian context, this should include support for vaccine registration especially for those with access constraints.
- Clear, consistent and transparent communication regarding service availability, risks, and benefits through general as well as intensive campaigns with
- Engagement of community leaders, celebrities, as well as health and scientific experts to build awareness, and
- Tailoring messaging according to health, scientific and general literacy of sub-populations using traditional and social media, as appropriate.
Related People:
- Dr Devaki Nambiar, Program Head – Health Systems and Equity, The George Institute for Global Health
- Sandeep Moola, Research Fellow, The George Institute for Global Health
- Nachiket Gudi, Consultant, The George Institute for Global Health